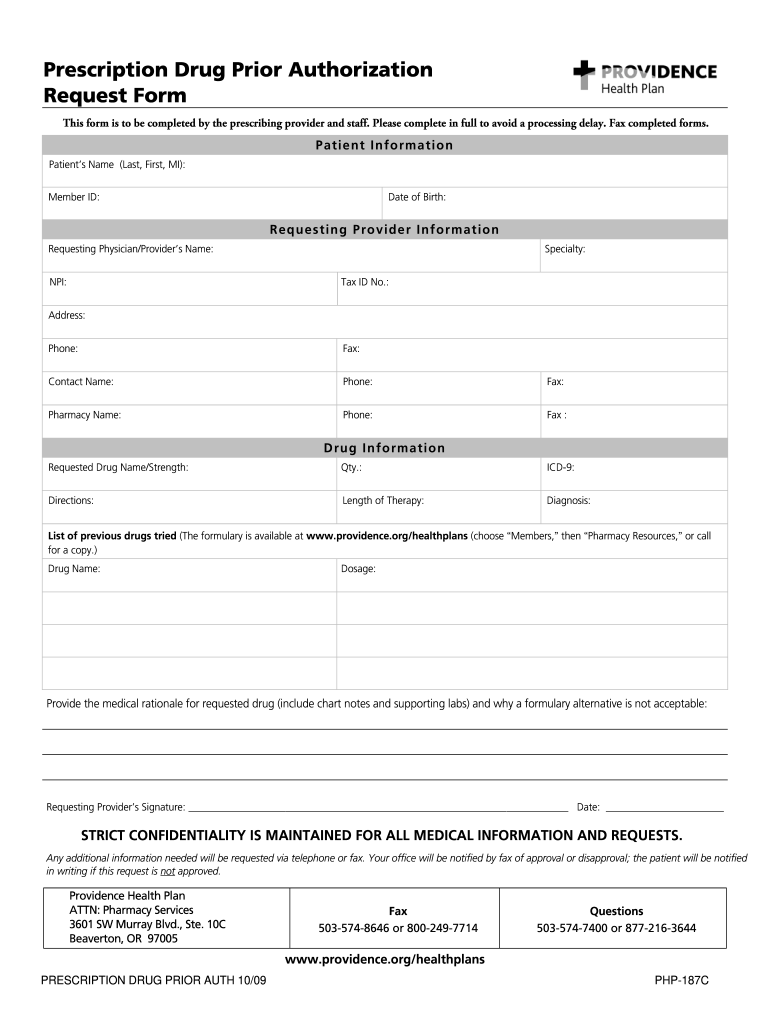
The Providence Health Plan Provider Appeal Form is a document that allows healthcare providers to appeal decisions made by Providence Health Plan regarding coverage, reimbursement, or other issues. This form is used to request a review of a denied claim or any other decision that negatively impacts a provider’s ability to deliver care to patients.
Providers can use the appeal form to present additional information, documentation, or arguments to support their case and potentially overturn the initial decision made by Providence Health Plan. It is an essential tool for providers to advocate for their patients and ensure that they receive the necessary care and services.
Providence Health Plan Provider Appeal Form
How to Submit the Providence Health Plan Provider Appeal Form
To submit the Providence Health Plan Provider Appeal Form, providers must carefully follow the instructions provided on the form. Typically, the form will require providers to provide their contact information, patient information, details of the denied claim or decision, and any supporting documentation.
Once completed, providers can submit the appeal form either electronically through the Providence Health Plan provider portal or by mail to the address specified on the form. It is essential to ensure that all required fields are filled out accurately and that any supporting documents are included to strengthen the appeal.
Benefits of Using the Providence Health Plan Provider Appeal Form
By utilizing the Providence Health Plan Provider Appeal Form, providers can effectively challenge decisions that may impact their ability to provide quality care to their patients. The appeal process allows for a fair review of the circumstances surrounding the denied claim or decision, giving providers the opportunity to present their case and potentially reverse the decision.
Additionally, submitting an appeal demonstrates a provider’s commitment to advocating for their patients and ensuring that they receive the care they need. It can also help providers strengthen their relationship with Providence Health Plan by showing a willingness to work collaboratively to address issues and find resolution.