When a patient is discharged from the hospital, it is crucial to ensure a smooth transition back to their home or another care setting. Hospital discharge planning forms play a significant role in this process by documenting important information about the patient’s medical history, medications, and follow-up care instructions. These forms help healthcare providers coordinate care and communicate effectively with the patient’s primary care physician and other healthcare professionals involved in their post-hospitalization care.
By using hospital discharge planning forms, healthcare providers can ensure that patients receive the necessary support and follow-up care to prevent readmissions and complications. These forms also help patients and their families understand their care plan and responsibilities, leading to improved patient outcomes and satisfaction.
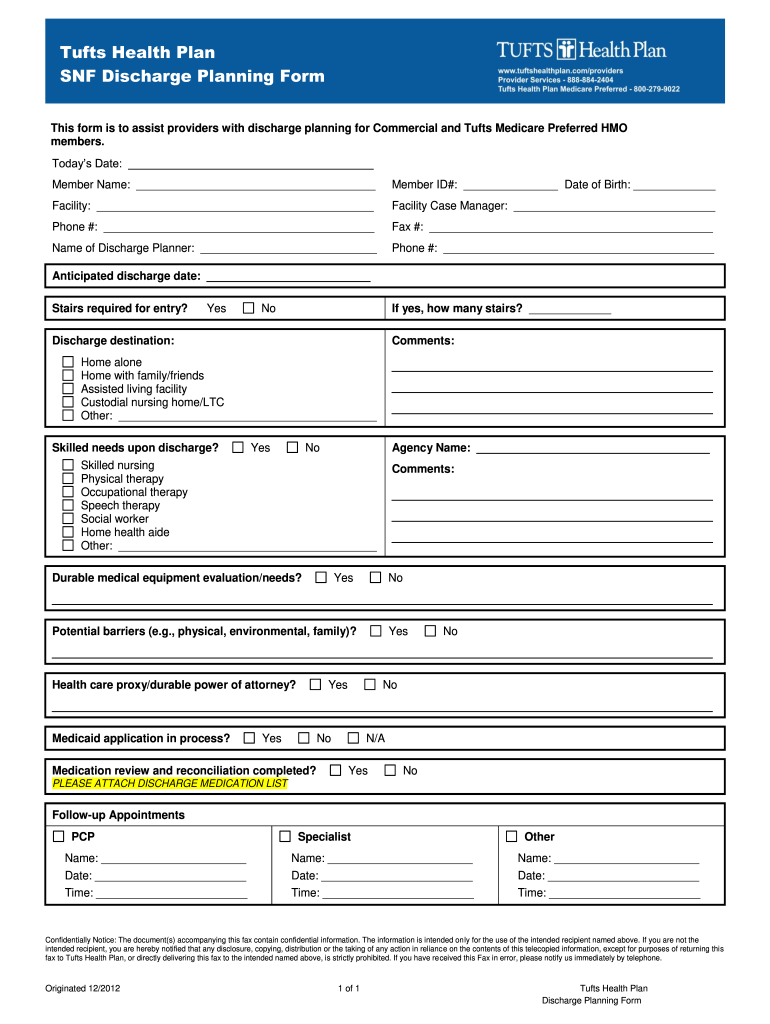
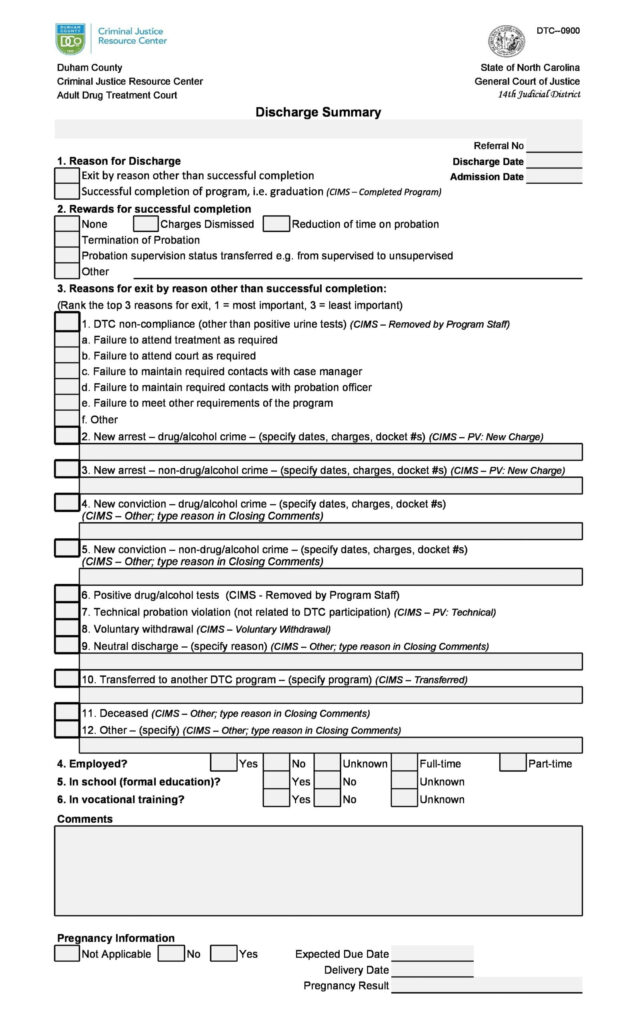
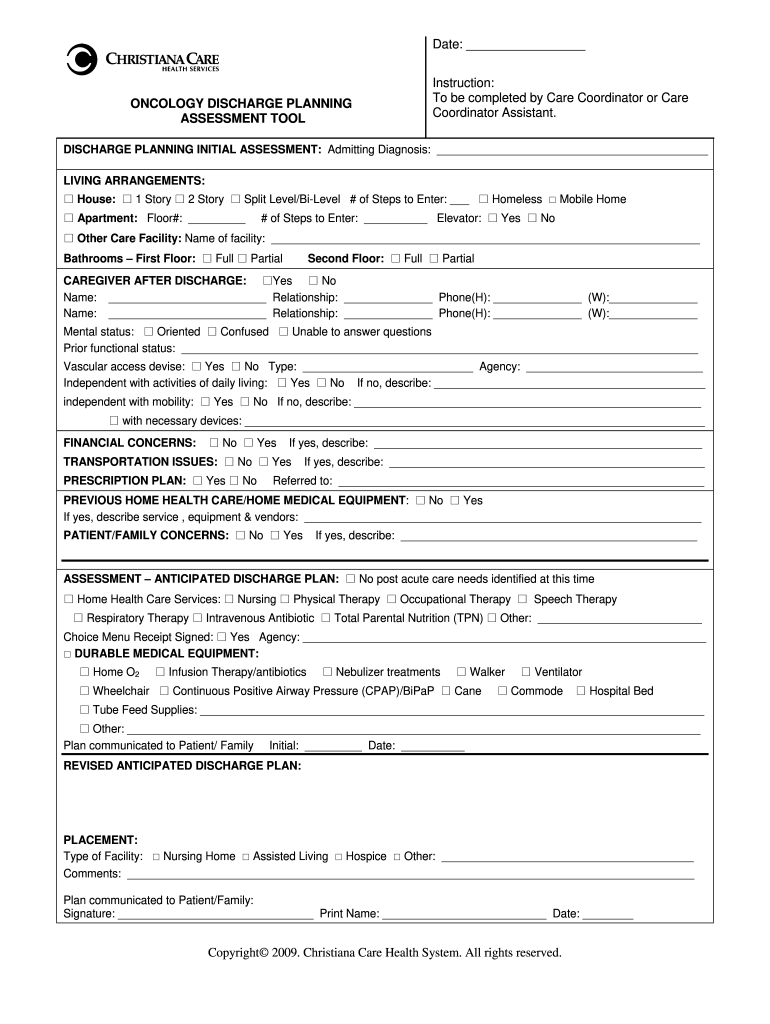
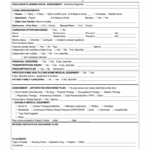
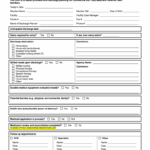
Hospital Discharge Planning Forms
Key Components of Hospital Discharge Planning Forms
Hospital discharge planning forms typically include essential information such as the patient’s diagnosis, treatment plan, medications, and any special instructions for post-discharge care. They also outline follow-up appointments, referrals to specialists, and home health services that may be necessary for the patient’s recovery.
Additionally, hospital discharge planning forms may include information on potential red flags or warning signs that patients and their caregivers should watch for after discharge. This proactive approach helps prevent complications and allows for prompt intervention if needed, reducing the risk of readmissions and adverse outcomes.
The Role of Technology in Improving Hospital Discharge Planning
Advancements in technology have made it easier for healthcare providers to streamline the hospital discharge planning process. Electronic health record systems allow for seamless communication and sharing of information between different healthcare settings, ensuring that all providers involved in the patient’s care have access to the most up-to-date information.
By incorporating electronic hospital discharge planning forms into their workflow, healthcare providers can save time, reduce errors, and improve the overall quality of care for patients. These forms can be customized to meet the unique needs of each patient and can be easily updated as their care plan evolves.
In conclusion, hospital discharge planning forms are a vital tool in ensuring a successful transition from hospital to home for patients. By documenting important information, coordinating care, and communicating effectively with all members of the healthcare team, these forms help improve patient outcomes and reduce the risk of readmissions. With the help of technology, healthcare providers can further enhance the efficiency and effectiveness of the hospital discharge planning process, ultimately leading to better care for patients.
Download Hospital Discharge Planning Forms
Discharge Planning Worksheet Pdf Fill Out Sign Online DocHub
Discharge Planning Form Fill Out Sign Online DocHub